Projects:2020s1-2413 Smart Sock for Aiding Prothesis Fit and Preventing Pressure Sores in Leg Amputees
Welcome to the wiki page for the 2020 Project Smart Sock for Aiding Prothesis Fit and Preventing Pressure Sores in Leg Amputees. This project has been undertaken as a part of Honours Research by students studying a Bachelor of Electrical and Electronic Engineering (Biomedical) at The University of Adelaide.
Contents
1.Introduction
The goal of this project is the analysis of data from array pressure sensors and the presentation of said data in a concise manner to both a layman user and a clinician. This is the programming of an android app and a pseudo prosthetic setup along with an array of pressure sensors to measure the pressure difference and location of pressure peaks and lows across the residual limb caused by the wearing of a prosthesis. This is of interest to clinicians and patients due to the pressure difference causing health complications in patients and unnecessary wear and tear on the prosthetic itself. To achieve this goal the team will design and implement both the graphical user interface(GUI) and the data analysis.
The project will demonstrate the knowledge that the team has learned over the duration of their study at the university and their ability to implement it.
2.Background
There are more than 8000 lower limb amputations performed in Australia every year according to Limbs4life Australian statistics. Due the amputations, many patients opt for using prosthetic so they can attempt to lead a normal life and be able to do normal daily activities such as walking, running and even intense activities such as hiking. Over the years, it has been discovered that it is of utmost importance that the residual limb and prosthetic socket fit is accurate since it very crucial to a patient’s health and comfort. According to multiple studies, a misfit between a residual limb and a prosthetic socket is the major cause for improper function, patient discomfort, skin breakdown, skin ulcers, edema, dermatitis and sometimes limb abandonment. This project aims to measure the, pressure difference between the residual limb and prosthetic socket, which causes patients to develop pressure sores and the preceding health problems discussed above. This project will be about developing a system which would assist clinicians and patients to identify the high-pressure points between the prosthetic and residual limb and make adjustments to have a better prosthetic fit which would eventually ease patients of some discomfort.
2.1 Technical
The two most common types of sockets for a below the knee or transtibial amputation Patellar Tendon Bearing (PTB) and Total surface bearing (TSB). The PTB sockets tend to have an “indentation” at the PT region of the limb which bears the highest pressure from total body weight. The TSB sockets on the other hand work to distribute the weight evenly all over the residual limb. However, patients still tend to complain about discomfort due to pressure ulcers, skin ulcers and irritation. In this section of the paper, some already existing pressure measurement between a residual limb and prosthetic techniques will be discussed. The different methods of measurements may be have been used for prosthetic modification or just simply for a research paper. The four most used measurement techniques are F-socket, Strain Gauge pressure transducers, Finite Element Analysis & Fibre Bragg Grating Sensors. This section also includes some not so popular and new methods.
2.1.1 Tekscan Pressure Management Systems
One of the more popular techniques, F-socket pressure system & F-scan pressure system by the American company Tekscan which aims to measure the pressure between a socket and residual limb to assist in improving design, fitting , function and comfort of the prosthetic limb .
2.1.1.1 F-scan System
In a study conducted by some researchers from University of Strathclyde , measured the dynamic residual limb & prosthetic socket interface pressure of 90% of area within a transtibial prosthetic socket using 4 Tekscan F-socket transducer arrays. The first advantage of using this Tekscan system is that the transducer configuration does not interfere with the clinical use of the prosthesis, meaning no holes are needed to be drilled and tapped into the prosthetic socket to fit the transducer. The second advantage is that the strength of the F-scan system lies in the number of pressure cells recorded, instead of the data from an individual cell, this helps avoid inaccuracies. Four prosthetic socket transducer arrays were placed inside the patient prosthetic socket, this is to ensure the procedure had an identical placement and direct, accurate comparisons could be done. The transducers were of a total of 350 individual sensing points and the data was sampled at 150 Hz, which resulted in over 50,000 pressure measurements for a one single prosthetic step . This ensured promising final results and to be able to measure the pressure interface. A total of 48 patients from a hospital in Glasgow volunteered to take part in this study, out of which 24 were transtibial amputees. The limitation with this pressure measurement system was hysteresis, drift susceptibility to curvature and temperature, crosstalk, loading range and rate. This problem was overcome following rigid protocol to precondition, equilibrate and calibrate the sensor array before being use for the experiment . The F-scan system calculates the data from individual transducer cells on the four arrays and displays the average pressure for each of the four transducer arrays for each time frame.
2.1.1.2 F-socket System (in socket-sensor mat)
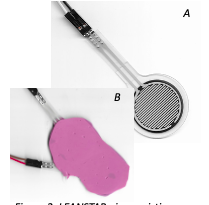
One technique used to measure pressure interface between residual limb and prosthetic is using in socket sensor mat or in this case the F-socket system by Tekscan. This sort of sensor is paper thin and can be placed between the limb and the prosthetic to get an accurate representation of the pressure difference along the region of the two surfaces and identify which are the high-pressure points . One such system known as F-Socket by the company Tekscan which uses their in-socket sensor mat to measure the pressure . This is done using force-sensitive resistive sensors (FSR) which are along a series of stripes which measure the static and dynamic pressure inside the socket. However, the downside to this is that since the sensor is paper thin, there is always a chance it may break, wrinkle or malfunction while being worn by the patient or during a research [4,36]. According to, this technique also has chances of non-linearity, hysteresis, drift, and susceptibility to electromagnetic interferences which casts doubts in the results. Another major downside to the F-socket system is its costing, a Single leg unit is $12,400 and double leg unit is approximately $17,200 . The F-socket sensor dimensions are 76.2mm x 203.2mm, with thickness of 0.28mm and it contains 96 sensors over an area of 161.3 mm2, and it is arranged into 6 columns and 16 rows.
2.1.2 Fiber Bragg Grating Sensors (FBG)
FBG sensors have been considered superior compared to other measurement techniques such as ( F-socket, SG transducers and FEM) because of their small size, light weight, flexibility, safety, multiplexing capabilities, high accuracy & sensitivity, high spatial resolution and electromagnetic interference immunity. An experiment conducted with FBG sensors in 2013, with no human subjects but researchers have attempted to mimic real life circumstances where they used real stump from an amputee and they used a heavy balloon with a thick wall.The balloon was placed into the prosthetic socket and inflated to a known pressure, since this was a very efficient way to calibrate the stump/socket pressure sensor and also test the FBG sensor performance and capability of producing repeatable patterns. The balloon was inserted into the socket where the FBG was already embedded and it was also attached to a pipe with an air compressor , which contained a pressure gauge to indicate the pressure being applied to the balloon. This experiment was conducted in seven trials and the average values were used to investigate the FBG behavior and this indicated that the FBG was sensitive to small changes in applied fore . According to, promising results were attained for an accurate pressure measurement which has led to a better socket fit and the patient satisfaction. The final results showed a good sensitivity and hysteresis and it also satisfied the requirement of being able to correctly measure the pressure applied to the Patellar Tendon region. In another study by the same researchers as the one discussed above, took their own design further and improved the FBG sensor to conduct another test, however in this one as well there were no human subject, instead researchers have tried to mimic an actual limb containing muscles, skins, tibia and fibula using silicon and plastic polyester resin . In this experiment F-socket sensor mats and FBG sensor results were examined to see which one showed more promising results. A machine was designed by the researcher which mimicked the patient’s gait cycle, to account for no human subjects in the experiment. Both F-socket sensing mats and the FBG sensors were calibrated before the experiment was conducted . The pressure profile was determined as a function of the recorded wavelength shifts . A LABVIEW software was used to process the wavelength of the reflected spectrum at a sampling frequency of 50Hz for each FBG sensor . When the gait stimulating machine was started, the sensor determined the back reflected wavelength in real time and on the other hand the F-socket sensing mat recorded the pressure interface between the residual limb replica to give the overall pressure distribution. FBG sensors has shown good linearity in this experiment with good hysteresis, accuracy, and precision. FBG sensors are considered to reduce the amount of non-linearity which occur from the F-socket sensing mats. However, the FBG sensors must be tested in actual human subjects to rule them over the F-socket sensing mats, but the initial trials have showed great results.
2.1.3 Mechanical
A common way of identifying areas of high and low pressure is the use of a substance such as lipstick or blue tack. By coating the inside of the socket and making the user wear it it; the pressure spread out the substance in such a way that high and low pressure areas can be identified. This does not allow for the identification of the time that pressure has occurred and areas of interest can be erased by subsequent movements of the patient.
2.2 Application
There currently doesn’t exist a mobile application that performs all the required functions. Most individual requirements of the application already exist as separate components. The tools to design them exist and can easily be accessed.
There are multiple coding environments that could be used to code the application. A list of some that were considered are shown below.
- Android Studio:
- A comprehensive environment that primary codes in Java but has support for the C family of languages.
- Extensive range of tools and coding example
- Requires Java.
- MIT App Inventor:
- a limited environment that is coded using a block visual style.
- This is the quickest method that requires the least amount of background research.
- Has support for Bluetooth Low Energy
- Visual Studio:
- A multi platform coding environment
- Extensive documentation and examples
- Has multiple versions with different licenses.
In the end due to the simpler coding that MIT App Inventor provided, it was chosen as the environment that would be used for the project.
3.Research Question
The research question for the project is: “Developing a system which would assist clinicians and patients identify high-pressure sore points in between residual limb and prosthetic stump”
4.Research Methods
To successfully undertake the project the team followed these steps.
- Identification of technology gap
- Interview with stakeholders
- Brainstorming of possible solutions
- Analysis of solutions and grading based on fulfillment of requirements and available budget
- Design of prototype and testing methods.
- Acceptance of design by stakeholders
- Construction of prototype
- Testing of Prototype
- Discussion of results
5.Design
5.1 Identification of purpose
The prototype that was deigned fulfills two major tasks:
- The real time monitoring of pressure distributions across areas of interest
- The gathering of pressure data in the daily routines of the user.
To achieve this we identified two major requirements
- Gathering of Pressure Data
- Mobility
Mobility
For mobility to be achieved the device needed to be small and light.
Pressure Gathering
For the gathering of pressure data, we first needed to identify the range of pressures that it would be under. To do this, Anthropometric Reference Data for Children and Adults: United States, 2003–2006, was used.
By approximating the residual limb to a cylinder with a hemisphere at one end and using the average calf and thigh circumferences, the total surface are was found.
Surface Area of Sides = 1/2*(Circumference/2π)*h
Hemisphere (without bottom) Surface Area = 2*π*(Circumference/2π)2
Then using the average weights the kg/cm2 was found.
5.2 System Design
The system was designed to be as simple as possible. This is shown in Figure 2.
5.3 App Design
The app was designed by creating a plan. The plan was reviewed by the stakeholders over multiple times, before it was finalised. Figure 3 shows the final design. The art is not final, but the app was coded to as closely resemble the design as possible.
6.Testing
The chosen sensors were attached together. Keeping the distance between them consistent. A simulation of the residual limb was created. This simulation is shown in Figure 5.
By measuring the changes in recorded pressure, the response of the system to stimuli was able to be identified.
7.Android Application
In order to present the data from the pressure sensors and easy to use android application was made as a part of the project. The android application was programmed using MIT APP Inventor, which is a visual block language. The first part of the project about designing a Graphical User Interface (GUI) for a layout of the app , after consulting with the internal stakeholders to get their feedback on what features would the doctors and patients benefit the most from through the app. The first GUI layout was made using FIGMA to get a general idea of what the final app would be looking like. The final app was simplified much more from the original idea, with the patients having the ability to navigate through the app to send their daily symptoms via email, text or voice recordings to their doctors straight form the app. The patients are notified of the appointments days before the due date and future updates to app includes any notes given to patients by the doctor is also updated on the app. Doctors are able to see the pressure measurements in terms of numbers and also in a graphical format to get a sound understanding of how prosthetic and residual limb pressures are changing over the area and impacting the patients. Patients can also see the pressure values through their apps. There is a FAQ section also included for ease of use for the users. Patients have a unique feature where the app tells the age of their prosthetic and keeps updating from the first date of log in by the patients. Future updates includes reminding patients for a prosthetic change appointment every 5 years or the recommended prosthetic usage periods by their clinicians.
There can be many more advanced features that can be added to the app, but due to the time restriction and the programming language used there were some cutbacks made so the team could have an outcome at the end. But this is a continuing project, meaning students who choose to do this project can work towards making a more advanced app as well as the physical prosthetic sock that could be worn by patients.
8.Virtual Ingenuity
Due to COVID-19, the original plans of having an in person ingenuity event was cancelled. Students were asked to prepare a poster and a 3 minute video to capture the essence of their project and reach out to the audience to describe how and why is this project helping the society.
9.Conclusion
The prototype demonstrates the feasibility of the design. More development should be undertaken and if budget permits array pressure sensors should be explored.
10.Project Team
10.1 Students
Nuzhat Farha
Marek Wojcik
10.2 Supervisor
Dr Said Al Sarawi
10.3 Stakeholders
Vivien Heng
Jane Morphett
Yiran Qu
11.Definitions and Abbreviations
12.References
[1]. "Australian statistics", Limbs4Life ~ empowering amputees. [Online]. Available: https://www.limbs4life.org.au/australian-statistics. [Accessed: 02- Jun- 2020].
[2]V. Rajtukova, R. Hudak, J. Zivcak, P. Halfarova and R. Kudrikova, "Pressure Distribution in Transtibial Prostheses Socket and the Stump Interface", Procedia Engineering, vol. 96, pp. 374-381, 2014. Available: 10.1016/j.proeng.2014.12.106 [Accessed 30 May 2020].
[3]E. Al-Fakih, N. Osman, A. Eshraghi and F. Adikan, "The Capability of Fiber Bragg Grating Sensors to Measure Amputees’ Trans-Tibial Stump/Socket Interface Pressures", Sensors, vol. 13, no. 8, pp. 10348-10357, 2013. Available: 10.3390/s130810348 [Accessed 18 April 2020].
[4]W. Carrigan, C. Nothnagle, P. Savant, F. Guo and M. B.J. Wijesundara, "Pneumatic Actuator Inserts for Interface Pressure Mapping and Fit Improvement in Lower Extremity Prosthetics", in June, International Conference on Biomedical Robotics and Biomechatronics (BioRob), Utown, Singapore, 2019, pp. 574-579.
[5]E. Al-Fakih, N. Abu Osman, F. Mahamd Adikan, A. Eshraghi and P. Jahanshahi, "Development and Validation of Fiber Bragg Grating Sensing Pad for Interface Pressure Measurements Within Prosthetic Sockets", IEEE Sensors Journal, vol. 16, no. 4, pp. 965-974, 2016. Available: 10.1109/jsen.2015.2495323 [Accessed 15 May 2020].
[6]"F-Socket System", Tekscan. [Online]. Available: https://www.tekscan.com/products-solutions/systems/f-socket-system. [Accessed: 01- Jun- 2020].
[7]T. Dumbleton et al., "Dynamic interface pressure distributions of two transtibial prosthetic socket concepts", Journal of Rehabilitation Research & Development, vol. 46, no. 3, pp. 405-416, 2009. [Accessed 20 April 2020].
[8]A. Polliack, R. Sieh, D. Craig, S. Landsberger, D. McNeil and E. Ayyappa, "Scientific validation of two commercial pressure sensor systems for prosthetic socket fit", Prosthetics and Orthotics International, vol. 24, no. 1, pp. 63-73, 2000. Available: 10.1080/03093640008726523 [Accessed 30 May 2020].
[9]McDowell, M., Fryar, C., Ogden, C. and Flegal, K., 2008. Anthropometric Reference Data for Children and Adults: United States, 2003–2006. National Health Statistics Reports, Number 10. Available at: <https://www.cdc.gov/nchs/data/nhsr/nhsr010.pdf> [Accessed 6 April 2020]
[10]D. Cronin, "Ballistic Gelatin Characterization and Constitutive Modeling", Ontario, 2011.
[11]A. Naylor, "Can Wood be used as a Bio-mechanical Substitute for Bone during Evaluation of Surgical Machining Tools?", BioResources, vol. 9, no. 4, 2014.